Implants – What is an implant?

Topic overview
Find out about “Fixed teeth in one day – the All-On-Four method”

Read or print a complete article on one page: Dental implants 
Introduction
One of the main focuses of our practice is dental implants. Dr. Schulte has been treating patients with implants since 1986 and has placed well over 3000 implants to date. As a specialist in oral surgery he has followed the evolution of this relatively young discipline with active interest from the very beginning.
Until not so long ago, patients with missing teeth had only two alternatives: If there were still two healthy adjacent teeth, these were filed down and a bridge fitted. But often enough the patients had to make do with a removable partial denture or even with full dentures. Apart from the unsatisfactory cosmetic result and the sometimes poor chewing function it is important to remember that removable dentures often constitute a serious psychological problem for the patient.
Fortunately, with dental implants it is now possible in most cases to provide patients with permanent fixed restorations which look and feel just like natural teeth. The latest studies show that implants placed by an experienced implantologist have long-term success rates of 95%. This means that ten years after the implantation 95% of the implants are still fully functional. These long-term results are even considerably better than those obtained with conventional bridges or partial dentures. Today it is considered that properly inserted implants can last a lifetime. For this reason we give our patients a ten-year guarantee against implant loss.
In recent years implantology has undergone enormous development. From new diagnostic procedures such as cone beam volumetric tomography (CBCT), to computer guided navigation for implant placement and immediate loading of the implants there are a number of new developments which promise the patient even more safety and comfort. However, unfortunately the big promises made in advertising and the media are not always fulfilled. On the booming implantology market there are also some dubious players around and it is not always easy for patients to separate the wheat from the chaff.
In order to give you a factual overview of the possibilities and limits of dental implantology, this chapter contains extensive and illustrated information that you can read in sections or download and print out as a PDF.

Dr. Markus Schulte is a specialist in oral surgery and implantology and has placed thousands of implants in over 30 years of professional practice.
What is an implant
A dental implant is an artificial tooth root made from a biocompatible (tissue-friendly) material that is inserted operatively into the jawbone to replace one or more missing teeth. Standard implants today are screw-shaped or cylindrical and made from pure titanium. Titanium is a unique metal: it fuses directly with the bone without an intermediate layer. This intimate contact between the bone and titanium is called osseointegration. Pure titanium is so tissue-friendly that it is not rejected by the body and does not trigger allergic reactions or inflammation of the gums. On account of its excellent biocompatibility, this hard and durable metal is widely used for other medical implants, too, e.g. for artificial hip joints, cardiac pacemakers etc. The titanium surface of dental implants is roughened by special processes in order to facilitate attachment of the bone cells and accelerate incorporation into bone.

The dental implants used today are usually cylindrical or slightly conical screws (the shape of the tooth root) and normally 6-18 mm long and 3-6 mm in diameter. In the head of the implant is a small internal screw thread for attachment of the support post (known as the abutment). Depending on the use (crowns, bridges, dentures) there are various kinds of abutments.
There are innumerable implant manufacturers on the market but only few systems are supported by scientific studies and long-term results. In our practice we use implants from the following manufacturers:
These manufacturers are market leaders with decades of experience and continuously improved systems backed by excellent long-term results.


Ceramic Implants
Recently ceramic implants are often promoted as an alternative to titanium. In contrast to titanium implants they are white, but in our opinion this is not a relevant advantage since the implant is placed inside the bone anyway and is therefore not visible.
A disadvantage, however, is that for reasons of stability ceramic implants can currently often only be made in one piece. This means that it is not possible to work with angulated abutments, which can lead to cosmetic and functional problems in the prosthetic treatment. The excellent biocompatibility of ceramic is another argument put forward in favour of this material. However, as pure titanium is also extremely biocompatible and there have been no reports of titanium allergy anywhere in the world, we do not see this as a relevant advantage of ceramic either. Moreover, ceramic implants are usually considerably more expensive than titanium ones. However, the chief reason why we do not currently use ceramic implants is the absence of reliable long-term scientific studies on fracture strength, behaviour in the bone etc. As we do not want to use our patients as “guinea pigs” for materials which have not been sufficiently tested, we will for the time being continue to use the titanium screw implants which have proved themselves millions of times over.
We refrain from using alternative implant forms such as leaf implants or BOI implants (Basal Osseointegration Implants) for the same reasons. Most professional associations do not recommend these implants either.

How is an implant placed?
The placement of dental implants is a surgical intervention performed under sterile conditions. The operation takes between about 30 and 60 minutes depending on the complexity, possibly longer if several implants are placed in one session. It is normally done under local anaesthesia and is absolutely painless. However, we know that even though there is no pain, many patients find such procedures stressful. Therefore in our practice we often use sedation, e.g. withlaughing gas (nitrous oxide) or other sedatives, in addition to the local anaesthetic. The benefit of this is that the patient feels fully relaxed and comfortable throughout the procedure.
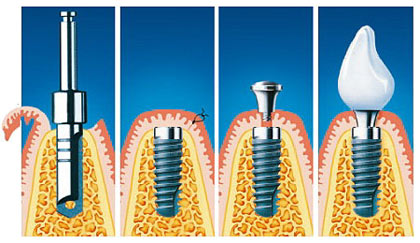
From left to right:
1. Drilling the pilot hole in the bone
2. The implant has been inserted and the gum tissue repositioned over the implant and secured with sutures
3. At the end of the healing phase (osseointegration), the gum tissue is opened again, an impression is taken and a healing screw inserted
4. The finished crown on the implant
Careful planning is the first step preceding an implant operation. The examination of the patient begins with careful inspection of the oral cavity and palpation of the jawbones. X-rays are taken to determine the available height of the bone. In straightforward cases it is sufficient to take a panoramic X-ray of the entire mouth (orthopantomogram, abbreviated OPG or OPT), possibly complemented by small dental X-rays taken inside the mouth.
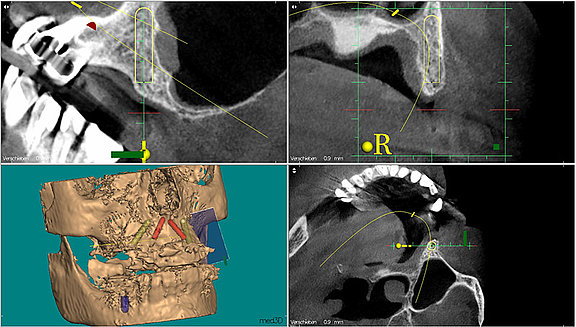
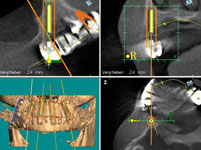
In more difficult cases in which the amount of available bone is limited and we have to operate in the proximity of sensory nerves, for example, we have a computed tomographic (CT) scan of the jaw done. Cone beam volumetric tomography (CBVT or DVT) is a new type of computed tomography which has been developed specially for the head region. In comparison to normal computed tomography CBVT involves up to 80% less radiation exposure. The radiation dose of CBVT is therefore approximately the same as that of a normal panoramic X-ray (OPG). You can find further information on X-rays and CBVT here.
Another option, particularly for larger operations such as bone augmentation or full-mouth reconstruction, is treatment under general anaesthesia. Treatment under general anaesthesia can be performed in our own operation theatre, in which case we call in an experienced team of anaesthesiologists.
As soon as the local anaesthetic has taken effect the gum is carefully opened. With a sequence of calibrated burs, the implant bed in the bone is prepared. To prevent overheating of the bone, preparation is done with sterile water cooling. The suitable implant is chosen and carefully inserted. The gum tissue is replaced over the implant and secured with sutures (stitches) and a provisional denture or bridge is fitted. In the case of template guided implantation the operation can be even performed as a closed procedure, that means without cutting open the gum tissue at all.
Computed tomography or cone beam volumetric tomography produces precise three-dimensional images of the jawbone on a 1:1 scale and permits optimal planning of the implant operation. The three-dimensional imaging permits exact measurement of the amount of available bone. The optimal positioning, length and diameter of the implants can now be planned on the basis of the available bone, as well as any necessary bone augmentation. The images also give us information about the quality of the bone (solid or porous). The CT or CBCT images also show the exact position of the nerves running through the bone as well as other structures which we must be careful to avoid injuring during the operation. This means considerable extra safety for the patient.
A further use of the three-dimensional images is for computer guided implantation, which is the safest and least traumatic method of all for the patient.
Uncovering the implant
Normally dental implants should be left to heal for 6-12 weeks without being loaded, except in the case of what is known as immediate loading. After the healing phase, a small procedure is performed to uncover the head of the implant. We often do this by laser because this guarantees particularly good wound healing and is painless for the patient. After uncovering the implant head we take an impression or intraoral scan and send it to the dental laboratory where the reconstructions (bridge, crown or dentures) are fabricated. Today, in many cases we choose an open (transgingival) healing of the implants, which does not require surgical uncovering.
Single-tooth implant
If a single tooth is missing and replaced by an implant we call this a single-tooth implant. In the past a gap caused by a single missing tooth was usually closed by a bridge. The filing down of the adjacent teeth that this involves is not necessarily a good idea, particularly if these are healthy teeth with no signs of tooth decay. It can sometimes result in the death of the tooth nerve (dental pulp) and a consequent need for root canal treatment. Also, the crown margins often provoke gum recession with poor cosmetic results.


In the case of a single-tooth implant the missing tooth is replaced by an implant which is inserted in place of the lost dental root. During the healing phase of usually a few weeks the implant remains under the gums without loading. During this time the patient can wear a provisional prosthesis which can be either removable or fixed (e.g. adhesive bridge). After uncovering the implant and taking an impression the crown that has been made in the dental laboratory is attached to the implant.
If a tooth has to be extracted, the implantation can be performed at the same time as the extraction. This is called an immediate implant. This spares the patient an additional visit and is a standard procedure today. Only in some cases, e.g. in the case of an acute infection, is it better to first remove the tooth and wait until the gum and bone tissue has healed before placing the implant. If the implant is fitted with a firmly attached provisional crown immediately after implantation, this is called immediate loading. This procedure is, of course, particularly comfortable for the patient because he leaves the practice with a fixed tooth replacement and does not need a provisional bridge or denture. However, immediate loading is not possible or advisable in all cases and the implantologist needs experience to weigh up the potential benefits and risks in the individual case.
Case from our practice: Single- tooth implants
Our 27-year-old patient S.G. was dissatisfied with the cosmetic appearance of her front teeth. Her two lateral incisors had been missing since birth. On the right the corresponding milk tooth was still there, while on the left the canine tooth had taken the place of the missing incisor and the milk tooth was behind it. She was particularly unhappy about the gaps and the asymmetric gum contours. We removed the two milk teeth and replaced them with implants. We evened out the gum margins by surgically extending the crowns. After bleaching, we then installed all-ceramic crowns on the implants and provided the adjacent front teeth with ceramic veneers. The implant crowns are now indistinguishable from the natural teeth.

Case from our practice: single-tooth implants

This 48-year-old patient had lost both middle incisors a few years ago as a result of an accident and had since then been wearing a clasp-retained removable partial denture. As she was dissatisfied with her appearance and the fit of the denture, she came to see us about implant treatment. Unfortunately, through the accident and the long time without teeth a lot of bone had already been lost.

After bone and gum augmentation and placement of two implants, all four incisors were provided with all-ceramic crowns. The natural cosmetic appearance of the front teeth is restored.
The alternative to a single-tooth implant is still a conventional bridge supported by the adjacent teeth. This is an option particularly if the teeth on either side of the gap are already crowned, have large fillings or are decayed and would need crown treatment anyway. In the case of healthy teeth with no tooth decay the preferred solution today is definitely implants, which can be fitted without having to file down healthy teeth. A three-unit bridge costs approximately the same as a simple single-tooth implant with crown.
Alternative to a single-tooth implant
The alternative to a single-tooth implant is still a conventional bridge supported by adjacent teeth. This is an option particularly if the teeth on either side of the gap are already crowned, have large fillings or are decayed and would need crown treatment anyway. In the case of healthy teeth with no tooth decay the preferred solution today is definitely implants, which can be fitted without haveing to file down healthy teeth. A three-unit bridge costs approximately the same as a simple single-tooth implant with crown.
Bridges: Advantages and Disadvantages

+ No operation necessary
+ Good aesthetic and functional results
- Adjacent teeth have to be filed down
- This can lead to death of the tooth never (dental pulp)
- Cannot be extended if further teeth are lost
- Tooth decay and gum recession at the crown margin possible
- Bone loss due to missing tooth
- Oral hygiene more difficult
Implants: Advantages and Disadvantages

+ No need to file down adjacent teeth
+ Extendable
+ Oral hygiene same as for natural teeth
+ Implant prevents bone loss
+ No tooth decay possible
- Requires a surgical procedure
- Surgery is more elaborate if bone or gum augmentation is necessary
Implants for larger gaps (partially edentulous jaw)
If there are several teeth missing we speak of a partially edentulous jaw. In the past, when a bridge was not possible, a removable partial denture was often the only option. These dentures partially cover the roof of the mouth (palate) and can impair speech or trigger a gag reflex in sensitive patients. With implants the gap can be closed with an implant-supported fixed bridge, without removable dentures and without having to file down healthy adjacent teeth. Cosmetic appearance and chewing function are excellent with implant-retained bridges in comparison with clasp-retained removable dentures.
Dental prosthetics yesterday
Missing teeth in the upper and lower jaw are replaced with clasp-retained removable dentures (cast partial dentures). These partially cover the roof of the mouth and do not offer optimal chewing function and cosmetic appearance.

Dental prosthetics today
The back teeth of the lower jaw on both sides are replaced with natural looking, fixed ceramic bridges and crowns on implants.

Partial dentures: Advantages and disadvantages
+ Simple clasp-retained dentures less expensive
+ No surgery necessary
- Poor aesthetic appearance, e. g. due to visible clasps
- Sometimes unsatisfactory fit
- Bar or plate can be uncomfortable
- Clasps can damage the supporting teeth
Implant bridges: Advantages and disadvantages
+ Optimal chewing function and aesthetic appearance
+ Feel just like natural teeth
+ No retainers, plates or bars necessary
+ No damage to adjacent teeth
- Surgical procedure necessary
- More expensive than simple removable partial dentures
Toothless (edentulous) jaw and full-mouth reconstruction with implants

In the past the loss of all teeth inevitably meant wearing full dentures with all the associated consequences: pressure sores, often poor fitting dentures, particularly in the lower jaw, limited chewing function, reduced sense of taste, sometimes gagging or impaired speech.
In addition, the continuous pressure of the dentures causes shrinkage of the jawbone due to accelerated bone loss (also known as bone resorption or atrophy) and thus leads to an even worse fit of the dentures. Poorly fitting dentures do not provide adequate support for the tissues of the face, particularly the lips, which makes the patients look older and encourages the development of premature wrinkles. The psychological effect should not be underestimated either as for many people full dentures symbolise old age.
With dental implants we can now break this vicious circle. Only 2-4 implants fitted with studs or other attachments are sufficient to give a full denture stable support. With more sophisticated constructions it is possible in most cases to anchor a fixed bridge in a completely toothless (edentulous) jaw. The old dream of new fixed teeth has now become reality and enables many people to regain an important piece of quality.
For many years now, one of our key areas of expertise has been the rehabilitation of toothless patients and full reconstruction in patients who have to have all their teeth removed. In the following we give you an overview of the most important methods used in our practice for removable and fixed dental restoration in toothless jaws.

Visibly improved quality of life: 57-year-old toothless patient before and after receiving fixed implant-supported replacement teeth. The good support for the lips and cheeks gives the face a fuller appearance and makes the patient look considerably younger.
Push-button prostheses
Removable dentures on implants
This is the simplest and often the least expensive form of implant treatment for toothless patients. It is suitable particularly for patients who are already wearing dentures but are dissatisfied with their fit. In the case of severe shrinkage of the jawbone – after wearing full dentures for years – removable implant-supported overdentures are sometimes preferable to a fixed restoration. Retainer elements (studs or bar) are screwed onto the implants inserted in the jaw and the dentures clip onto these and sit firmly.
Of course the dentures still have to be taken out and cleaned after meals. However, the good fit gives the patients a feeling of security and chewing is much more comfortable compared with normal full dentures. In the lower jaw at least two implants are needed, each of which is fitted with one stud. However, we prefer stud constructions with three implants because the denture is much more stable if it is anchored at three points and does not wobble or tilt even when biting with the incisors.


An alternative is the insertion of four implants which are connected with a bar made of a noble metal or titanium. The prosthesis then clips onto the bar with great precision. The advantage of bar-retained dentures is that they are immediately functional. Only one day after implantation the patient is given the dentures and can immediately chew normally with them; there is no long waiting for the implant to integrate. In the upper jaw we do not recommend studs for removable dentures but prefer bar-retained dentures on 4-6 implants. However, a fixed restoration with an implant bridge is usually better.
Bar prostheses
1st case study from our practice: Removable tooth replacement on implants
55-year-old patient after full reconstruction with 4 implants in the lower jaw and bar-anchored removable dentures. The firm hold of the dentures ensures comfortable chewing.


2nd case study from our practice: Removable tooth replacement on implants
This 39-year-old patient, a former photo model, had had major reconstruction done several years ago in Eastern Europe. All her teeth had been crowned. Unfortunately the work had been done so badly that the patient had developed massive periodontal disease and tooth decay under the crowns. When she came to see us she was suffering from severe depression because she was ashamed to show her teeth in public.
All the teeth in the upper jaw had to be removed. On account of the considerable bone loss we decided in this case to fit bar-retained dentures on 8 implants. The extractions, bone augmentation and implant placement were performed in the same session under general anesthesia.




Fixed implant bridges in the toothless jaw – Fixed teeth in one day

More and more patients today want implant treatment which does not involve removable dentures but provides “permanent teeth” which look and feel just like natural teeth. In the past, this kind of full reconstruction with dental implants was a very major procedure as it involved placing 6 to 8, sometimes 10 implants in each jaw, and bone augmentation was often also necessary. This meant that the treatment was very expensive and unaffordable for many patients. In addition, the whole treatment often took as long as 12 months, with tedious healing phases during which the patients had to put up with removable full dentures, before the final bridgework could at last be fitted.
Today, thanks to the advances in modern implantology we can offer our patients solutions which are considerably less time consuming, more comfortable, safer and less expensive.
With the All-on-4™ method we can provide immediate fixed tooth replacement with only four implants per jaw. The back implants are placed at an angle of 30-45 degrees. This means that we can usually manage without bone augmentation and allows us to steer clear of critical anatomical structures such as the maxillary sinus in the upper jaw and the sensory nerve in the lower jaw.
After placement of the 4 implants (any remaining teeth can be removed in the same session) a previously fabricated provisional bridge is screwed onto the implants. The patient leaves our practice with fixed functional teeth. About three months later the final bridge is then installed.
All scientific studies consistently show a very high success rate for implant bridges using the All-on-4™ technique. All-on-4™ bridges are just as durable and reliable as constructions with six or more implants. In addition, we can avoid bone augmentation, which is often stressful for the patient and not without risk, and can considerably reduce treatment times and costs. For all these reasons we prefer the All-on-4™ method for full reconstruction with implants. Because of our extensive experience with this method we are convinced of the longevity of the All-On-Four-prosthesis and grant our patients a 10 year guarantee against implant loss.
In the case of extreme bone loss in the upper jaw, e.g. after wearing full dentures for decades, there is sometimes no bone left at all and normal implantation is therefore impossible. A good alternative to extensive bone grafting is the zygomatic implant.
Further extensive information on fixed teeth in one day are available here.
Computer guided implantation:
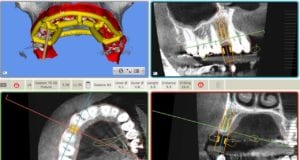
The digital data obtained in this virtual implantation are then used to prepare a three-dimensional template made of plastic or titanium. This drilling template is placed in the patient’s mouth during the implant operation. Drill sleeves in the template guide the bone drill during the implantation and ensure that the implants are placed exactly in the ideal position planned on the computer. The benefit for the patient is that the gums often do not have to be opened (no swelling, practically no pain after the procedure). A further advantage of template guided implantation is the possibility of preparing an exactly fitting provisional bridge before the implant placement. This means that ideally the patient can go home with fixed, functional teeth shortly after the implant placement. In order not to raise false expectations and give you honest information we should, however, mention that at the present time computer guided template implantation is not possible or appropriate in all cases. We always use this particularly safe and gentle method if it brings the patient concrete benefit.

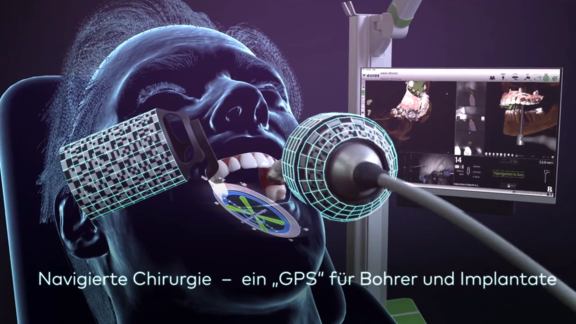
Dynamic computer-guided navigation: The X-Guide system
As one of the first practices in Switzerland, we are equipped with X-Guide, a system for dynamic navigated implantation. Two optical sensors, which are attached to the drill and to the patient’s jaw, enable free 3-D navigated surgery without any splints. The current position of the drill or implant is permanently displayed in three dimensions on the screen and compared with the previously planned ideal positioning.
In contrast to the rigid template-guided method, we can navigate freely with the X-Guide. Especially in the complex cases that we often treat, it is often necessary to deviate from the planning during the operation. The X-Guide gives us this possibility and therefore enables flexible and safe operation even in unpredictable situations.
Vorteilhaft für den Patienten ist, dass die Schleimhaut oft nicht einmal eröffnet werden muss (Keine Schwellung, kaum Schmerzen nach dem Eingriff). Ein weiterer Vorteil der computergeführten Implantation ist die Möglichkeit, bereits vor der Implantation eine passgenaue provisorische Brücke herzustellen. So können wir den Patienten im Idealfall kurz nach der Implantation mit festen, belastungsfähigen Zähnen versorgen und nach Hause entlassen. Um keine falschen Erwartungen zu wecken und im Sinne einer seriösen Information muss allerdings darauf hingewiesen werden, dass eine computergeführte Implantation derzeit nicht in allen Fällen möglich oder sinnvoll ist. Wir wenden diese besonders sichere und schonende Methode immer dann an, wenn sie dem Patienten konkrete Vorteile bringt.


Case study from our practice: Full-mouth reconstruction with computer guided implantology
This 84-year-old woman could no longer cope with her old, poorly fitting dentures and came to us for advice about fixed tooth replacement on implants. On account of the patient’s advanced age we wanted to offer her the least traumatic, minimally invasive procedure possible.




First we obtained a CT scan with X-ray films placed in the upper and lower jaws (cone beam computed tomography (CBCT) with particularly low radiation exposure) in order to perform a three-dimensional analysis of the available bone. The evaluation of these X-rays showed that there was sufficient bone mass for immediate implant placement without bone augmentation using the All-On-4-method.
The planning of the optimal positioning of the implants in the bone and the determination of the diameter and length of the implant were performed virtually on the computer using the Med3D® software. The digital data thus obtained were sent to a specialised dental laboratory which fitted the X-ray templates with highly precise drill sleeves which serve to guide the drilling and the implants into exactly the previously planned correct position during implantation.

Then the operation could be performed with local anaesthesia. The remaining pivot teeth were removed. Then the templates were fixed in the mouth, the implant drilling performed through the drill sleeves, and the implants placed in the planned position, again using the template. The great advantage of the computer guided implantology is that it is no longer necessary to first open the gums with a scalpel and expose a large area of bone. As the implant position has already been planned on the computer the drilling can be performed minimally invasively through the closed gum tissue and the implants placed in the drill holes. According to the all-on-4 method, four implants were placed in each jaw.




The operating time was thus considerably shortened to about 45 minutes per jaw. The swelling and pain normally observed after major implant operations were almost entirely absent, there was no bleeding or bruising either.
As the implant positioning had already been decided preoperatively (before the operation), the dental technician was able to make the provisional restorations before the implant placement. These bridges were screwed onto the implants immediately after the operation (immediate loading).
The patient was able to leave our practice with fixed tooth replacement on implants. The definitive All-On-4 bridges were fitted after three months.



Piezo-Chirurgie

Piezosurgery is a novel bone surgery technology developed by Prof. Tomaso Vercellotti that also opens up new horizons for dental implantology. Specially developed surgical instruments that utilize microvibrations at ultrasound frequencies allow extremely atraumatic bone cutting with minimal damage to tissue. The biggest advantage of Piezosurgery compared with the conventional scalpels, drills and burs used for cutting bone is its selective cut. This means the instrument cuts easily through hard tissue (bone) while soft tissue such as nerves, blood vessels or gum tissue remains undamaged even if it comes into direct contact with the tip of the instrument. Another advantage of Piezosurgery is that there is practically no bleeding, the bone is not traumatized and wound healing is therefore much better. We use this innovative technology mainly for taking bone grafts, for the sinus lift procedure and for all operations in which there is a danger of injuring nerves or blood vessels.
Further information on Piezosurgery.
PRP: Growth factors from the patient′s blood
A recent development in implantology is the administration of factors which stimulate bone growth. The aim of this strategy is to accelerate integration of the implants into the bone and thus shorten the often tedious healing phase (with provisional bridge or dentures) following implant placement
The platelet rich plasma (PRP) obtained from the patient’s blood contains high concentrations of a number of growth factors in addition to the platelets. These growth factors lead to good bone regeneration and help achieve faster and better wound healing particularly in high-risk patients (e.g. diabetics, smokers). In our practice we use the automatic PCCS system from the company 3i to obtain the PRP. The system requires only 60 ml of the patient’s blood to prepare the concentrate.
Zygomatic and pterygoid implants Immediate rehabilitation of the atrophic upper jaw
Zygoma implants and pterygoid implants are an interesting alternative to bone grafting in the case of severe bone loss in a toothless upper jaw. Special very long (about 50 mm) implants are anchored in the zygomatic bone or the pterygoid bone and used to support a fixed implant bridge. The bone volume of the zygomatic / pterygoid bone remains quite stable even when there is bone loss in the region of the jawbones. One can either combine two to four normal implants at the front with two zygoma implants or use four zygoma implants (two on each side), if necessary combined with two pterygoid implants. The bridge which is screwed onto the implants is then fitted using the All-On-4 method. If there is severe bone loss in the upper jaw, zygoma implants are the only means of providing immediate fixed tooth replacement without extensive bone grafting. The stress and risk of the operation are far less than in the case of major bone augmentation. Further advantages are the drastically shortened treatment times due to the possibility of immediate loading of the implants and the considerably lower cost as no bone grafting and no hospitalization are necessary.

Case study from our practice: Zygomatic Implants
This 56-year-old patient consulted us because she had serious problems with her poorly fitting removable upper dentures. The X-ray and CT scan showed massive bone loss (atrophy) in the upper jaw so that placement of implants would have required prior major bone augmentation. For this bone graft we would have had to take bone from the hip. This is quite a stressful procedure for the patient. After the bone graft patients have to remain in hospital for a few days and there is often some difficulty walking in the first weeks after the operation due to the bone removal from the hip. In addition, in the initial phase not even provisional dentures can be used so as not to jeopardize the integration of the grafted bone. Then, for about nine months after the procedure, only a provisional removable full denture can be worn. It should also be mentioned that such large bone grafts have a relatively high failure rate of about 15-20%.



After thorough discussion of all the options, our patient therefore decided on zygoma implants. In an outpatient operation under general anaesthesia we removed the remaining teeth from the upper jaw and stably anchored four zygoma implants, two on each side, in the zygomatic bone. On the very same day we were able to install a fixed provisional bridge on the implants. Three months later the definitive prosthetic rehabilitation was performed.
Here you can access further scientific information on zygomatic implants and pterygoid implants



Immediate implants
Immediate implantation (not to be confused with immediate loading) means that a tooth is extracted and replaced immediately with an implant in the same session. This spares the patient an additional operation and is a standard procedure today. However, sometimes, e.g. in the case of infected teeth, it is better to remove the tooth first and wait until the inflammation in the bone has subsided before placing the implant.
Immediate loading of implants
As described above, implant treatment traditionally consisted of several successive phases:
- Extracting the tooth
- Placing the implant
- Healing phase (6 weeks to 6 months)
- Uncovering the implant
- Installing the permanent crown, bridge or dentures
The long waiting time before completion of the final permanent restoration can be a problem, particularly if a satisfactory fixed provisional restoration cannot be fitted. In the case of major full-mouth reconstruction with implants, which involves removing all the teeth and replacing them with implants, the patients often had to wear full dentures for months until the implants had integrated and could be loaded.
In such cases, immediate loading of the dental implants can be particularly advantageous. In a single session (also under general anaesthesia), all teeth are removed, the implants placed and a provisional fixed bridge prepared which is screwed onto the implants some hours after the operation. This procedure offers a great gain in comfort and time for the patient. However, it is important to emphasise that immediate loading is only feasible if there is a sufficient bone mass and bone quality to ensure stable anchoring of the implants. If this is not the case, it is always advisable to leave the implants to integrate without loading and only install the restoration when this has taken place.
Case study from our practice: Immediate loading
54-year-old patient with severely compromised dentition. Periodontal gum disease and dental decay had led to such serious damage that it was no longer possible to save the teeth. The patient had suffered considerably from her cosmetic “disfigurement” and expressed a wish for full-mouth reconstruction under general anaesthesia with “permanent teeth” from the very beginning. It was important to her that she remained aesthetically presentable throughout the entire treatment period.



Under general anaesthesia all teeth in the upper and lower jaws were removed. In the same session we placed 4 implants per jaw. The All-On-4 method allows such stable anchoring of the implants in the bone that fixed, functional bridges can be installed immediately. On the same day, 4 hours after the operation the patient was fitted with fixed provisional bridges screwed onto the implants and was able to return to her home town. The definitive bridges were then fitted three months after the beginning of treatment.





Risks and complications of dental implants
Today dental implants have a very good long-term prognosis. More than 90% of implants placed by experienced implantologists are still in full service after ten years. These are figures which cannot be matched by other medical disciplines, if we think of hip replacement in orthopaedics for example. Nevertheless, even with the most careful planning and performance of the procedure failures can still occur. Overloading of the bone or bacterial infections can lead to failure of implants or bone augmentations, less often adjacent sensory nerves or dental roots may be damaged.
The main risk factors for implant failure are:
- poor oral hygiene
- heavy smoking
- marked bone loss in the jaw
- poorly controlled diabetes with fluctuating blood glucose levels
- reduced immunity, e.g. in patients taking immunosuppressants after organ transplantation or patients with severe rheumatoid arthritis or other autoimmune diseases
- Zustand nach Bestrahlung des Kiefers (Strahlentherapie bei Tumoren)
Regular check-ups and meticulous daily oral hygiene are the best prerequisites for lasting success of the implant treatment. If there is nevertheless implant failure, a renewed implantation can usually be performed after the bone has healed.
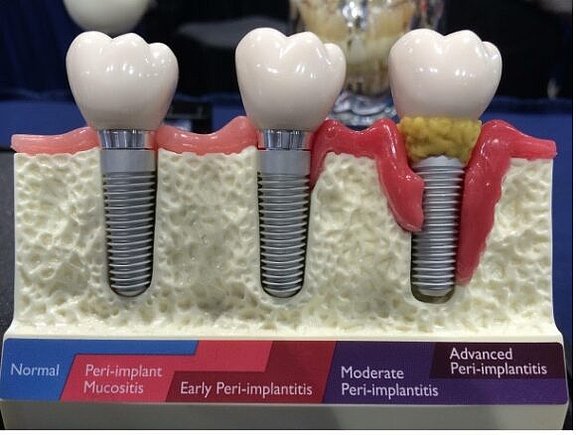
Peri-implantitis: Periodontitis around the implant
Summary:
- How can peri-implantitis be recognised and how does it progress?
- Risk factors for peri-implantitis
- Treating peri-implantitis
- Galvosurge: The new weapon against peri-implantitis
The same aggressive bacteria that are responsible for periodontitis in natural teeth can also attack implants and cause inflammation in the gums and bone around the implant. The technical term for this “implant inflammation” is peri-implantitis.
How can peri-implantitis be recognised and how does it progress?
It is treacherous that peri-implantitis (like periodontitis) remains painless for a long time and is therefore often only noticed late. In the early stages, inflammation of the gums around the implant (mucositis) is the first sign with redness and possibly slight swelling of the gum line with an increased tendency to bleed. Probing and measuring the gingival pockets usually reveals a slightly increased pocket depth. This inflammation of the gums (mucositis) is reversible, i.e. it can heal without consequences if it is treated locally and the cause is eliminated.
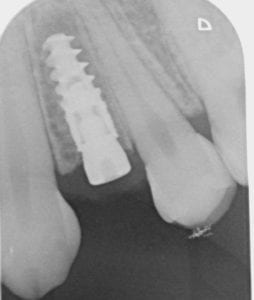
If the mucositis is not treated, it often turns into a “real” peri-implantitis with bone loss. The bacteria now attack the bone around the implant and break it down more and more (resorption). This creates a bone crater around the implant, which can only be detected with an X-ray, preferably an intraoral one. Sometimes you will also find some pus oozing out around the implant. The probing of the gum pockets at the affected implants now shows – depending on the bone loss – clearly increased values. Pain only occurs later – if at all – so that the inflammation often remains unnoticed for a long time.
If peri-implantitis is not treated, it always leads to the loss of the affected implant in the end.
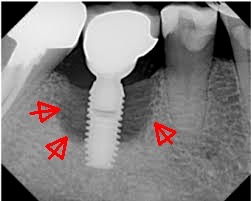
The X-ray shows a deep bone crater around the implant. As the patient, who did not come for regular check-ups, was not in pain, the inflammation was discovered by chance. Because of the already advanced bone loss, the implant had to be removed.
Peri-implantitis is not uncommon. As things stand today, it is assumed that about one third of all implants are affected by this inflammation in the course of a lifetime. Unfortunately, peri-implantitis is often only recognised late because it is initially painless. For all implant patients, regular check-ups with the dental hygienist are therefore essential. During this recall, the gum pockets are checked and X-rays are taken. In this way, inflammations at implants can be diagnosed in time and countermeasures can be taken.
What are the risk factors for peri-implantitis?
The following factors favour the occurrence of a peri-implant inflammation:
- Inadequate oral hygiene and lack of control
The presence of bacterial plaque in the mouth increases the risk of peri-implantitis. Therefore, implant patients should maintain optimal oral hygiene and have regular check-ups, usually every six months, as part of the dental hygiene recall. - Smoking
It is statistically proven that heavy smokers (more than ten cigarettes per day) have a significantly increased risk of implant inflammation. We therefore recommend that our implant patients stop smoking if possible. - Periodontitis
If a patient suffers from untreated periodontitis, the risk of peri-implantitis is increased. The reason is the massive concentration of aggressive periodontitis bacteria in the gum pockets. For this reason, periodontitis should first be treated before implants are placed. - Diabetes
Diabetes with poorly controlled or fluctuating blood sugar is a risk factor for many inflammations. Periodontitis and peri-implantitis are also more common in these patients. - Genetic predisposition
It is now known that certain genetic constellations on the IL-1 encoded genes significantly increase the risk of periodontitis and peri-implantitis. This is especially true if additional risk factors are present, e.g. smoking. - Medications
Cytostatic drugs, immunosuppressants and some anti-inflammatory drugs suppress the body’s natural immune response to bacterial infections and can therefore promote inflammation at implants. - Local factors
Improper placement of implants, e.g. without the required minimum distance from each other or from neighbouring teeth, can lead to peri-implantitis over time. The quality of the gum tissue around the implant also plays a role: it should be firmly attached and not moveable.
How to treat peri-implantitis
If the peri-implant inflammation is still confined to the mucosa, local treatment of the pocket can help. The dental hygienist cleans the implant surface and gently removes tartar and plaque. The bacterial biofilm can be gently removed with a powder jet device (Air Flow). With good oral hygiene, the mucositis can heal without consequences after the treatment. In some cases, repeated local treatments may be necessary.

The Air-Flow device uses a water-air jet that “shoots” a powder at high speed onto the surface to be cleaned. The particles consist of the amino acid glycine and are biodegradable. The implant surface is not roughened or damaged by this powder jet.
If peri-implantitis has already led to a bone defect, it is no longer reversible and, if left untreated, will progress to the loss of the implant. Therefore, a timely surgical revision is necessary. This involves opening the gums around the implant under local anaesthetic and exposing the bone. After removing the inflammatory tissue, the infected implant surface is decontaminated, i.e. freed from bacterial plaque. Special titanium brushes or powder jet devices can be used for this, but they often do not reach all points of the infected implant surface due to the depth of the bone crater. In our opinion, the best results are achieved with the new Galvosurge procedure. Exposed rough implant surfaces can also be smoothed and polished with small polishing instruments to prevent the accumulation of bacteria.
In some cases it is possible to fill the resulting bone defect with the patient’s own bone or bone substitute material and thus regenerate the lost bone.
Implant before and after bone augmentation. After decontamination of the implant with the Galvosurge device, the bone defect was filled with the patient’s own bone and bone substitute material and covered with a membrane. The picture on the right shows a perfectly regenerated bone one year later.
Galvosurge: The new weapon against peri-implantitis

A novel and promising method to combat peri-implantitis is the Galvosurge procedure developed in Switzerland. After exposure, an electrical voltage is applied to the implant and a special electrolyte cleaning liquid is sprayed onto the implant. According to the principle of electrolysis, hydrogen bubbles now form on the implant surface, which completely remove the bacterial biofilm even in inaccessible places.
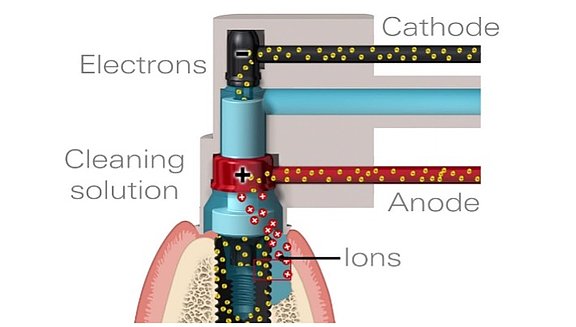

The Galvosurge principle: The implant is covered with an electrolyte solution. An electrical voltage applied to the implant causes gas bubbles to form on the metal surface, which completely eliminate the infected plaque (biofilm). This makes successful bone regeneration possible.
You can see a video about the Galvosurge principle here:
The first results of the Galvosurge treatment are extremely positive and show a real progress compared to the techniques used so far. We are pleased to be able to offer our patients this innovative method in our practice.
Questions and Answers about dental implants
The durability of implants has been studied for about 30 years in long-term studies. The results to date are encouraging and indicate that, with good oral hygiene and regular check-ups, implants placed by an experienced dental surgeon can last a lifetime.
Generally speaking, yes, except in the case of some rare diseases. Age is not relevant. Implants in older patients have the same good prognosis as in young patients. However, good oral hygiene is essential.
Advantages With implants it is possible to provide aesthetically pleasing fixed tooth replacement even in cases where in the past only removable bridges or dentures were possible. Another advantage is that, in contrast to bridges, it is not necessary to file down the adjacent teeth. Implants prevent bone loss and give full dentures firm anchorage.
Disadvantages The need for a surgical procedure can be perceived as a disadvantage, likewise the healing time for integration of the implants (except in the case of immediate loading). Implant treatments can also be more expensive than conventional dentures or bridges.
Before deciding on implant treatment the advantages and disadvantages of the treatment must be carefully weighed up in each individual case.
The procedure under local anaesthesia is completely painless. If desired, additional sedative medication (conscious sedation) can be given or the procedure can be performed under general anaesthesia. After the treatment it is normal to feel some soreness for a few days. This can easily be controlled with pain medication. Some more or less marked swelling for 3-5 days is also normal, sometimes there can be bruising but it will fade rapidly.
The healing time required before an implant can be loaded depends on the bone quality and the number, length and diameter of the implants. In ideal cases when several stable implants are involved immediate loading is sometimes even possible. Otherwise it is normally necessary to wait 6-12 weeks before the implants can be uncovered and loaded. If bone augmentation is necessary, the healing period can be as long as 6 months or so. We usually make a provisional tooth replacement before implant placement which can normally be fitted immediately after the operation so that the patient is not without teeth at any time.
No, implant supported bridges are possible in which missing teeth can be replaced by bridge elements. If all the teeth are missing or have to be extracted it is often sufficient to place four implants to support a complete bridge with 12 teeth (All-On-Four).
The statutory health insurance funds in Switzerland generally only pay for dental treatment with or without implants in exceptional cases if the tooth damage was caused by serious medical conditions. Click here for further information on costs and insurance cover.
As the procedure can be performed painlessly with local anaesthesia, general anaesthesia is not usually necessary for simple implant placement. General anaesthesia is only indicated in the case of more major operations involving implants in both jaws and bone augmentation. However, many patients prefer not to be conscious during their treatment and therefore choose treatment under general anaesthesia which we offer as an option. A good alternative is sometimes additional sedation with medication or laughing gas in addition to the local anaesthesia. This is known as conscious sedation. For detailed explanations on the topic of general anaesthesia and sedation click here.
This depends on the extent of the operation. After a single-tooth implantation you can normally go back to work immediately. After larger operations you should take it easy for 2-3 days.
Young people implants can only be placed when jaw growth is complete, that is from about the age of 18 years. In adults there is no upper age limit. Statistically, implants in older people are just as successful as in young people as the ability of the bone to integrate the implant does not decline with increasing age. However, meticulous oral hygiene is essential.
Normally, when we talk of bone loss we mean osteoporosis, a condition which occurs particularly in women after menopause and in which the bone loses its stability. Osteoporosis can also affect the jawbone. However, in most cases implantation is possible even with osteoporosis. It may be necessary to place more implants to support larger bridges and to allow a longer healing period in order to prevent overloading.
Sometimes we also talk of bone loss when we mean local loss of bone in the mouth, e.g. after periodontal gum disease or in toothless parts of the jaw. This kind of bone loss is also called atrophy. If there is insufficient bone for implantation as a result of atrophy bone augmentation can help. We also use methods which permit implant placement without bone grafting even in a toothless jaw with extreme atrophy (zygoma-implant).
Today we know that heavy smokers (more than 10 cigarettes per day) have a higher risk of losing implants than non-smokers. Smoking suppresses the body’s local mechanisms for fighting off harmful bacteria with appropriate antibodies. This means that smokers are more likely than non-smokers to develop bone loss around their natural teeth (periodontal disease) or implants (peri-implant disease). In particular after major operations with bone augmentation smokers have a definitely higher risk of complications. We therefore advise our smoking patients to give up smoking before implant treatment.
Titanium is an extremely biocompatible material which does not cause a foreign body reaction in the bone. There are no reports of allergy to titanium either. A genuine rejection reaction is therefore not possible. Loosening or failure of implants is due to overloading of the bone (e.g. too short a healing time, poor bone quality) or bacterial infections but not to rejection by the body.
There are innumerable implant manufacturers on the market but only few systems are supported by long-term scientific studies. We use implants from the companies Straumann, Nobel Biocare and 3i that are supported by excellent documentation. Furthermore, these market leaders guarantee the component supply even after many years. This is extremely important when, for example, we need to replace a connecting screw after ten years.
As we all know, advertising claims often have little to do with reality. The immediate loading of implants, meaning the immediate attachment of a fixed tooth replacement to freshly placed implants, has considerable benefits for the patient: chewing is significantly more comfortable during the healing phase, there is no need for removable provisional bridgework and a significant time saving. However, in each individual case these benefits must be weighed up against the potential risks, which should not be underestimated. It is also important that the implantologist has extensive experience with immediate loading of implants. In our practice we use this method in selected cases in which the benefits for the patient clearly outweigh the risks.
The rules for implants are basically the same as for natural teeth: Good oral hygiene is recommended and pays. The use of dental floss and interdental brushes is helpful for keeping the area between the implants clean. Our experienced dental hygienists will be happy to help you and give you instructions about proper use of the various dental care products.
Additional information on “Fixed teeth in one day – the All-On-Four technique”

