Wisdom Teeth
The rearmost teeth of the upper and lower jaw (counting from the middle outwards, tooth number eight) are called wisdom teeth. When fully exposed (they usually appear between eighteen and thirty years of age) and correctly aligned, and with enough space in the jaw, these teeth can be useful masticatory units. However, surgical removal must be considered if this is not the case. The older the patient, the more difficult this operation can be. To avoid complications, surgery should not be unnecessarily delayed.
Read or print a complete article on one page:Wisdom Teeth
If you are interested in specific topics or if you want to read the chapter in sections, please choose from the following bullet points:
When should the wisdom teeth be removed?
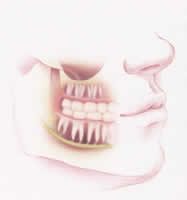
The jaw of many patients is not large enough to cope with additional wisdom teeth. Insufficient jaw space and false axis alignment (displacement) of the tooth bud often impede the breakthrough of wisdom teeth. They remain partially or completely embedded in the jawbone and never reach the occlusal plane. Depending on whether or not the teeth break through the gum, one refers to partially impacted or impacted wisdom teeth.


The risk of caries and infection

caries in the posterior part of the second
lower molar. The reason for this is a
not timely distant, horizontally
displaced white tooth.
Oral hygiene of partially impacted wisdom teeth is often difficult. The result is often carious decay of the wisdom tooth or even the neighbouring second molar. In the same way, this can lead to chronic gingivitis or painful abscesses where the tooth breaks through.
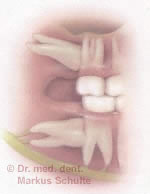
Cysts

displaced white teeth. The findings
were collected randomly during a
routine radiograph.
Impacted wisdom teeth are often the cause of cysts. A cyst is a cavity filled with fluid, which can develop unnoticed and thereby destroy the jawbone. In rare cases, a cyst can also develop into a tumour.
Orthodontic indications
The thrust of erupting wisdom teeth sometimes can cause displacement of the dental arch resulting in cramping of the anterior teeth. Wisdom teeth may also need to be extracted before orthodontic treatment.
Facial pain
Displaced wisdom teeth sometimes can cause neuralgic-like pains in the facial area and thus must be removed.
Prosthetic indications
Impacted wisdom teeth should be removed before making extensive prosthetic restorations (bridges, full or partial dentures).
At what age should wisdom teeth be removed?
Progressive root growth and constantly densifying jawbone makes extracting wisdom teeth at an older age more difficult. Therefore, the surgical removal of wisdom teeth should take place at an early age, as soon as it becomes clear the wisdom teeth will not break through correctly. The risk of resulting complications for juveniles is fairly small, as wounds have a tendency to heal well. Jawbone and gums heal rapidly, with almost no lasting defects.
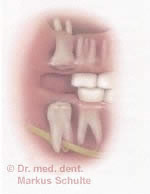
The operation
Firstly, an extensive preoperative examination is carried out. The X-Ray examination (orthopantomography) shows the wisdom teeth and the root form, the position within the jawbone, and the proximity to certain anatomic structures (nerves, maxillary sinus).In some cases, e.g. if the root tips overlap the sensitive nerve of the lower lip, a cone beam (3D) radiograph is required to assess the difficulty and risk of surgery. We can produce these 3D images with our in-house CBCT X-Ray machine. The results of the examination are discussed with the patient and a treatment plan drawn up. For the correct evaluation of the state of health in the face of the planned operation and anaesthetic, we require extensive information about notable allergies, general illnesses or current medication.

Before the tooth is extracted, the mucous membrane is opened, revealing the tooth hidden below. Any covering bone is carefully removed. Then the tooth is extracted, either as a whole or piece-by-piece, and the wound is stitched closed. The operation takes between twenty and forty-five minutes, depending on the complexity. A post-operative examination of the wound is made the day after surgery; the stitches are removed one week later.
Anaesthesia methods
The removal of displaced wisdom teeth is a routine outpatient operation, usually carried out under local anaesthesia. The operation may be painless; it is nonetheless a strenuous procedure for anxious patients. For this reason we regularly use conscious sedation with nitrous oxide. During surgery, the patient breathes a mix of laughing gas and oxygen through a small nasal mask. This easily controllable, reliable and safe method brings complete relaxation and loss of anxiety while still fully conscious. There are no unpleasant after-effects, and most patients find it a pleasant experience. A further alternative is surgery under intravenous twilight sedation or general anaesthesia. In our clinic we have a modern operating theatre and an expert team of anaesthesiologists at our disposal. This alternative is especially practical when removing several displaced wisdom teeth in one session.
Post-operative - what is to be expected?
Dr. Schulte and his team will explain exactly how you should behave after the operation. You will receive all necessary medication and an appropriate information leaflet.
Pain: the duration and intensity of the pain experienced depends on the complexity and scale of the operation. As a rule, any pain felt is not pronounced and subsides after a few days. The painkilling medication provided allows you to cope with this problem easily.
Swelling: you can expect a more or less distinct swelling as a result of this operation. Cold compresses help reduce swelling, which should reach its peak around forty-eight hours after surgery.
Haematoma/bruising: temporary bruising as a result of haematoma sometimes occurs. Impeded mouth opening: The ability to open the mouth is restricted within the first few days of the healing process.
Risks and complications
The surgical extraction of wisdom teeth is a routine procedure carried out regularly, without complications, at our dental office. The more experience the surgeon has, the less likely complications are. Nevertheless, the patient’s comprehensive education includes information about possible outcomes, however uncommon they may be.
- Infections: As with any operation, there is a risk of wound infection. Local treatment (wound irrigation, drainage) and, if applicable, administering antibiotics, will provide a fast cure. Should your condition worsen unexpectedly, please inform us immediately.
- Maxillary sinus: Extracting long rooted upper wisdom teeth or a high bud position can lead to an open maxillary sinus. A tight suture is routine, the wound usually heals without complications.
- Neighbouring teeth: The roots of neighbouring teeth are occasionally damaged when in immediate vicinity of the wisdom teeth.
- Paraesthesia: The sensitive nerves of the tongue and lower lip are in immediate anatomical relation to the lower wisdom teeth. Rarely, there may be temporary loss or dysfunction of feeling in the tongue or lower lip. Permanent dysfunctions are extremely rare.
- Fracture of the jaw: In rare cases, If the jawbone is weak (osteoporosis, atrophy, particularly extensive bone loss), there is a risk of fracturing. In either case, sporting activities and hard food should be avoided in the first few weeks after surgery.
- Root remnants: Wisdom teeth with long, slender roots may lose their tips during surgery. These remnants are usually located and meticulously removed from the jawbone. Should the removal of these remnants represent an unusual risk (for example, near nerves), they can be left in place; this has no negative effect on the healing process.